How Hemiplegic Migraine is Closely Related to Upper Motor Neuron Lesions
Posted on January 29 2024,
At first glance, the pathophysiology of migraine, which includes cortical spreading depression, may appear to be significantly distinct from upper motor neuron lesions that are seen in pathologies like multiple sclerosis, amyotrophic lateral sclerosis, physical trauma, infectious diseases, etc., but at a functional level, they have much in common. In fact, I will prove that, at a functional level, migraine has more in relation to an upper motor neuron lesion than any other pathology.
But, first, let’s define some terms. Cortical spreading depression (CSD) is a wave of neuronal and glial depolarization that spreads across the brain cortex (depending on which part of the brain the CSD involves, a patient with migraine may experience visual, sensory, aphasic aura, or motor aura in the case of hemiplegic migraine). Therefore, CSD is an electrical phenomenon that results in temporarily inactive neurons.
Upper motor neurons (UMNs) are the cortical neurons responsible for sending signals from the primary motor cortex, down the brain and into the spinal cord to initiate voluntary movement. Stroke, spinal cord injury, motor neuron disease, and other neurological conditions can damage UMNs, disrupting the transmission of descending signals to lower motor neurons that control the skeletal muscles. We can already see one glaring similarity- both interrupt signaling from cortical areas to the spinal cord.

To make this comparison properly, let’s use hemiplegic migraine as it causes motor weakness due to CSD. While -plegic may indicate paralysis, most attacks are motor weakness. Therefore, patients must have motor weakness for a diagnosis of hemiplegic migraine. You can see the diagnostic criteria below:

Motor symptoms often start in the hand and spread up the arm and face. They are usually unilateral (sometimes switching sides during the same migraine flare or even between flares) or bilateral which is seen in 1/3rd of cases in familial hemiplegic migraine (FHM).
As we stated earlier, it is cortical spreading depression that causes the motor weakness and other aura symptoms that must accompany hemiplegic migraine for a diagnosis.
It's called "cortical" because it occurs in the cortex, which is the outermost layer of the brain.
It's called "spreading" because there is a wave of depolarization that spreads out from an initial point.
It’s called “depression” due to the disruption of brain activity.
As this wave spreads into different cortical regions, it can cause aura symptoms. For example, if it spreads into the visual cortex, it could cause visual aura.
And to reiterate, CSD describes this spreading wave of disrupted cellular activity in the brain's cortex that is believed to directly correlate with the aura phase and other symptoms of a migraine flare. The areas whose function is temporarily disrupted by the CSD wave determines what types of aura symptoms someone experiences.
So, cortical spreading depression occurs in hemiplegic migraine where it must cause (according to the diagnostic criteria) traditional aura symptoms like visual, sensory, and/or speech/language symptoms, but it also must cause motor weakness.
How do CSD and UMN lesions cause arm weakness?
Our journey begins in the outermost gray matter of the cerebrum known as the cerebral cortex. Conscious motor signals arise within the frontal cerebral cortex located anterior to a prominent fissure in the brain known as the central sulcus.
The central sulcus divides the frontal lobe from the parietal lobe and demarcates a crucial cortical region—the primary motor cortex. It is within this primary motor strip that descending motor commands initiating voluntary movement are spawned.
Now, the best theory we have on the map of the primary motor cortex is the motor homunculus, but that may change as it has recently been contested, but, in general, various body parts align to defined sections of the motor cortex.

From these cortical origins, upper motor neurons descend together, forming a thick fan-shaped bundle called the corona radiata. The fibers then converge, passing through a critical structure situated between the thalamus and basal ganglia named the internal capsule. It is here that the pathways for the corticospinal and corticobulbar tracts diverge temporarily.

The corticospinal tract traverses the capsule through the posterior limb, while the corticobulbar tract travels via the genu or bend of the capsule- that is just the back end. Both motor routes then descend further into the brainstem. Midbrain, pons, and medulla are the 3 sections that make up the brainstem in descending order.
As the fibers descend from the internal capsule into the midbrain, they funnel through and consolidate within cerebral peduncles. These paired structures make up a portion of the midbrain. The peduncles serve almost like highways, allowing passage of the descending connections between the higher motor processing centers and the spinal cord below.
It is in the midbrain that we have the first corticobulbar extensions split toward their target cranial nerves. However, we will only concern ourselves with CN VII, which is the facial nerve.
So, now we are at the pons. Let’s continue with the corticospinal tract, however, even though that’s where the facial nerve finally matters. We will get to the facial nerve after we finish the corticospinal tract.
The corticospinal fibers descend through the medulla. Most pass through two medial pyramids named the medullary pyramids. These landmarks are the reason why you may see the corticobulbar and corticospinal tracts also being referred to as the pyramidal tract.
Reaching the junction between the medulla oblongata and spinal cord, a major crossover of fibers occurs called decussations. Here approximately 85-90% of the corticospinal tract fibers decussate, extending across the midline to the opposite lateral white matter of the spinal cord. They form the lateral corticospinal tract controlling distal limb movements before synapsing on lower motor neurons.
The remaining anterior corticospinal tract fibers controlling axial trunk muscles cross over at spinal levels.
Why does this matter?
In hemiplegic migraine, there is usually unilateral, contralateral motor weakness.
So, the CSD goes across a hemisphere impacting the primary motor cortex. As I said before, another aura is needed so it can also go across the occipital cortex causing visual aura and so on and so forth, but it must go through the primary motor cortex. This causes weakness on the contralateral side of the body.
This is also how upper motor neuron lesions work. Any lesion in the corticospinal or corticobulbar tract above the decussation results in a contralateral issue. If there is a lesion below the side of decussation, then the motor weakness will occur on the same side. Therefore, because CSD impacts the corticospinal and corticobulbar tract at the highest possible level, the cortex, then it causes contralateral weakness.
Now, let’s go back to the pons to talk about the facial nerve that diverged from the corticospinal tract at this position (it is part of the corticobulbar tract).

The facial nucleus in the pons contains neurons that innervate upper and lower facial muscles separately. The upper half of the nucleus controls the upper facial muscles, while the lower half controls the lower part of the face.
A key point is that the upper facial nucleus receives bilateral input from both left and right hemispheres, but the lower nucleus only gets input from the opposite cortex. Therefore, a cortical lesion only knocks out input to the opposite lower facial muscles. Although weaker, the patient can still move the upper facial muscles due to preserved same-side cortical input. This results in contralateral lower facial weakness but retained ability to close the eyes or raise the eyebrows.
In contrast, a lesion to the facial nucleus itself affects all the nerve fibers leaving that area. This removes input to both upper and lower facial muscles on that side. The result is full ipsilateral facial paralysis.
Let’s go through this again:
For the upper parts of the face, projections come from both hemispheres. So, for the forehead and orbicularis oculi muscles around the eyes, the LMNs receive input from both the left and right motor cortices.
UMN lesions generally spare the forehead. The main impact is on the lower opposite half of the face. In contrast, LMN lesions affect all the muscles on that half of the face equally, including the forehead.
When it comes to CSD, this is the equivalent of an upper motor neuron lesion as it impacts the cerebral cortex. When it comes to hemiplegic migraine, there is ipsilateral weakness in the hands that climb up the arm and may eventually reach the face due to the CSD. When it does reach the face, it spares the forehead (if unilateral) because it is an UMN issue. It’s a cerebral cortex issue. The cortex is still providing ipsilateral input.
With Bell's palsy a lower motor neuron (LMN) problem, the hallmark symptom is sudden and complete unilateral facial weakness. Therefore, it includes the forehead. There is no sparing of the forehead. The key diagnostic feature of bell’s palsy is isolated unilateral facial weakness without other neurologic symptoms. With UMN lesions, there are other symptoms that are also common with hemiplegic migraine.
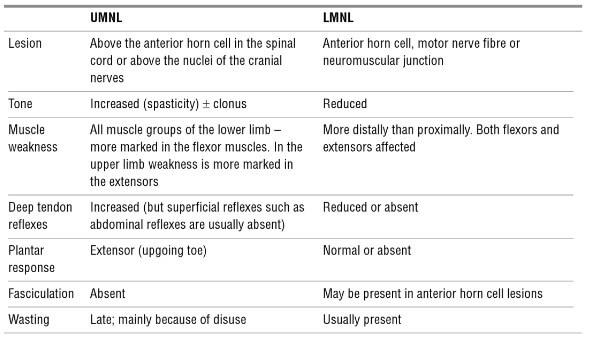
Hemiplegic migraine patients may experience hyperreflexia with clonus and a Babinski sign (a result of assessing the plantar reflex response).
Babinski sign video:
https://youtube.com/shorts/uthf0cWkkDk
You illicit a Babinski sign when you test the plantar reflex. As you can see in the video above, this involves using an object to firmly scrape the sole of the foot from the heel to the little toe and then inward along the arch.
An upgoing Babinski's sign is always abnormal in adults. Normal is usually flexion or curling of the toes. So, it’s abnormal in this video and this indicates an UMN pathology somewhere along the corticospinal tract from the cerebral cortex down to the spinal cord.
And the quick reason for hyperreflexia with clonus is due to the fact that the brain is what modulates the reflex arc and doesn’t allow it to overextend. Without it, there is hyperreflexia because the reflex doesn’t need to go to the brain, it only needs a lower motor neuron.
Hyperreflexia with clonus video:
So, in summary, at a functional level CSD and UMN lesions share these similarities:
1. Interruption of signaling from motor cortical areas to spinal cord.
2. Paralysis or weakness below level of impact/injury.
3. Weakness is contralateral to impacted hemisphere.
4. May cause hyperreflexia with clonus and a positive Babinski sign
However, with CSD, this is temporary, and the person usually regains normal function. With UMN lesions, the loss is usually permanent unless there is regeneration or neuroplasticity is taken into account. Moreover, CSD does not only impact the primary motor cortex, but goes across the entire cerebral hemisphere impacting many more areas.
Fri, Apr 18, 25
Weather Conditions & Migraine Attacks: Is there a relationship?
This meta-analysis found that weather conditions, especially temperature and ambient pressure changes as well as increased levels of certain air pollutants (PM10, PM2.5, NO2, CO, and O3), are significantly associated...
Read MoreFri, Apr 18, 25
Understanding the Link Between Endometriosis and Migraine
Understanding the Link Between Endometriosis and Migraine: New systematic review and meta-analysis reveals a significant connection between these two conditions and what it means for patients.
Read More

