New Study Unravels the Complex Relationship Between Migraine and Sleep
Posted on March 06 2024,
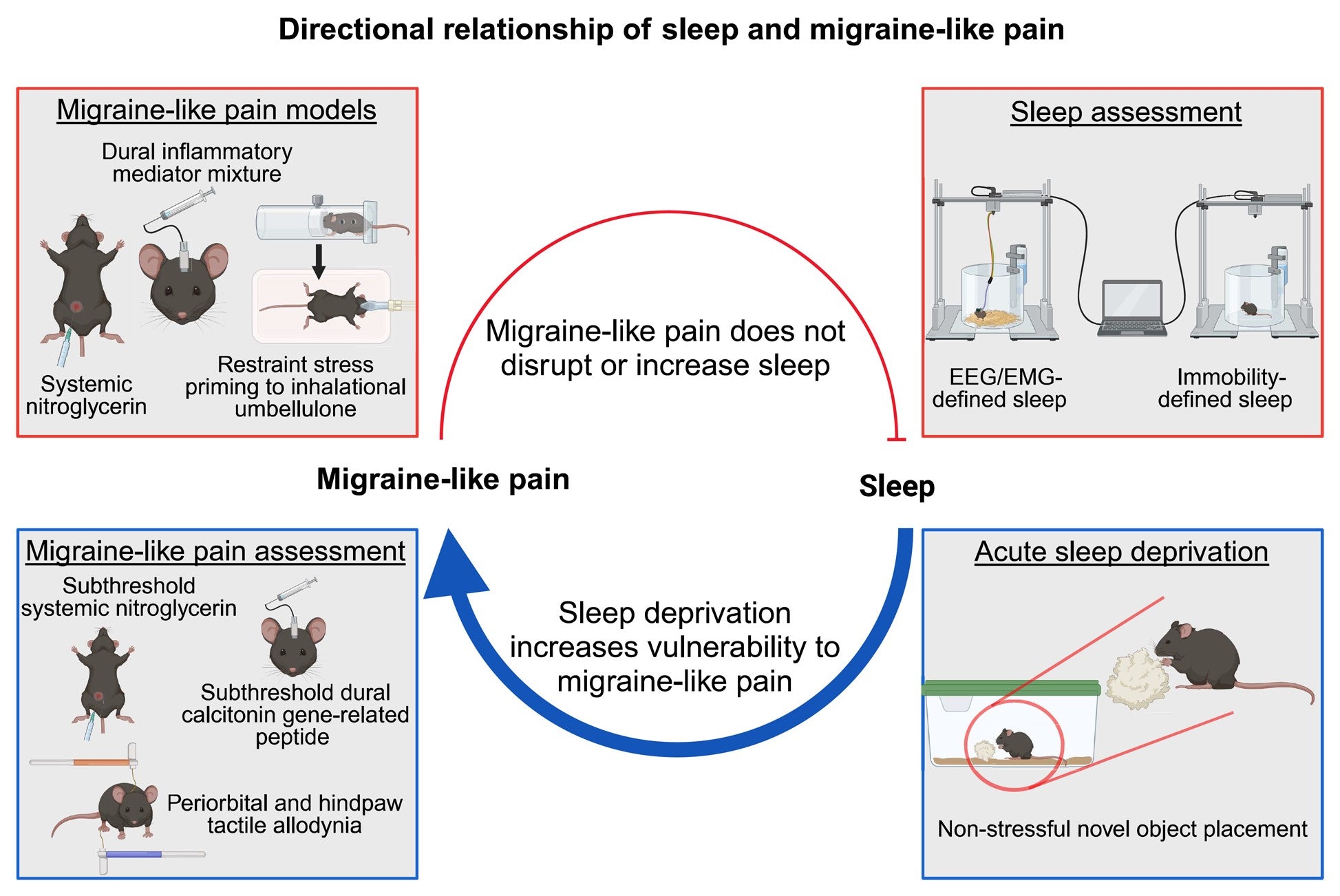
Migraine and sleep problems seem to go together, but which one causes the other? A new preclinical study from researchers at the University of Arizona has provided fascinating insights into the directional relationship between migraine pain and sleep disruption.
The Investigation
The research team took a multi-pronged approach to explore how migraine affects sleep and vice versa in mouse models. They induced migraine-like pain through different methods - systemic nitroglycerin injection, dural inflammatory soup application, and inhalation of umbellulone (a TRPA1 agonist) in primed mice. Sleep was monitored using both the gold standard electroencephalogram (EEG)/electromyography (EMG) recordings as well as a non-invasive immobility tracking method.
The Surprising Findings
Contrary to what many patients with migraine report experiencing (and we will get to this later), the study found that acute and chronic migraine-like pain did not disrupt the mice's sleep quantity, architecture (sleep stages), or depth. Neither nitroglycerin-induced migraine pain, inflammatory dural activation, nor umbellulone in the primed model affected total sleep time or sleep quality measures like non-rapid eye movement (NREM) and rapid eye movement (REM) sleep, regardless of whether pain was induced during the sleep or awake phase.
However, the reverse relationship unveiled a fascinating discovery. While migraine-like pain did not disturb sleep, sleep deprivation increased the vulnerability to migraine attacks. Using a novel object exposure method that did not increase stress markers, the researchers sleep deprived female mice for 6 hours. This single night of sleep deprivation did not directly cause migraine-like pain. However, when subsequently given subthreshold (normally ineffective) doses of nitroglycerin or the migraine peptide CGRP, the sleep-deprived mice developed robust periorbital (around the eyes) and hind paw allodynia (pain hypersensitivity) - hallmarks of migraine pain. This vulnerability persisted into the following day after acute sleep deprivation.
Implications
These findings suggest a directional link where sleep disruption may prime the system to increase susceptibility to migraine attacks. As the authors note, "Our data reveal that while migraine-like pain does not significantly disrupt sleep, sleep disruption increases vulnerability to migraine-like pain."
This has important implications for migraine management. Improving sleep quality through lifestyle changes, behavioral therapies like cognitive behavioral therapy for insomnia (CBT-I), or pharmacological approaches may help reduce the likelihood of migraine attacks in susceptible individuals.
Many migraine patients, including myself, use Cerebral Tranquility to combat this issue.
Moreover, prioritizing good sleep hygiene could be a valuable preventive strategy.
Limitations
Of course, migraine is a complex neurological disorder with many intricacies still to be uncovered. While this research provides valuable insight into the migraine-sleep link, it does have some limitations in fully reflecting the complex clinical experience of migraine patients. A combination of basic and clinical research will be needed to reconcile preclinical findings with patient reports and identify all crucial mechanisms disrupting sleep during migraine attacks.
This study suggests that migraine headaches do not impact sleep and only sleep decreases the threshold for migraine attacks. However, anecdotal, and personal experiences suggest migraine attacks do impact sleep. There can be several reasons for this discrepancy.
- Species differences. Mice may not fully recapitulate the human experience of migraine and its effects on sleep. The mechanisms linking migraine pain to sleep disturbances could involve higher-order processes not accurately modeled in rodents.
- Prodrome phase effects. The study focused on the headache phase of migraine attacks. However, in humans, the prodrome phase preceding head pain can involve symptoms like fatigue, difficulty concentrating, and mood changes which could potentially interfere with sleep, independent of pain.
- Multi-modal sensory hypersensitivity. During attacks, patients with migraine often experience heightened sensitivity to light, sound, smell, etc. This multi-modal sensory hypersensitivity, which was not assessed in the mouse models, could make it difficult for patients to fall/stay asleep despite optimal sleep environments.
- Comorbidities. Sleep issues in migraine patients may also arise from co-existing disorders like depression, anxiety, medication overuse/adaptation headache, etc., which were not factored into this study.
- Combination of the above.
For migraine patients plagued by sleep issues, these findings provide hope that addressing sleep problems could help keep the debilitating attacks at bay.
Wed, Apr 23, 25
Effectiveness and Tolerability of Atogepant (Qulipta) in the Prevention of Migraine
STAR study shows atogepant (Qulipta) effectively reduces migraine days by 56.6% in real-world clinical practice, even for patients with previous treatment failures. Learn about this breakthrough.
Read MoreWed, Apr 23, 25
Impact of Visual Stimulus Complexity on Associative Learning in Migraine Patients
Groundbreaking research reveals how migraine patients process visual information differently. This 2025 study found that migraine patients take longer to process simple visual stimuli compared to complex images, which is...
Read MoreSat, Apr 19, 25
FDA Authorizes First Digital Therapeutic for Migraine
In a development for migraine patients, the FDA has granted marketing authorization to CT-132, making it the first prescription digital therapeutic specifically designed for the preventive treatment of episodic migraine...
Read More
